Sleep apnea falls under the classification of ailments called sleep-disordered breathing (SDB). This classification includes upper airway resistance syndrome (UARS), snoring, obstructive sleep apnea, central sleep apnea and mixed sleep apnea. To understand sleep apnea, it’s important to consider the mechanics of respiration (i.e., the process of breathing), differences between the types of apnea, and the anatomy and physiology involving this condition.
What Is Obstructive Sleep Apnea?
Three simple exercises can help you educate patients about this chronic breathing disorder.
A diagnosis of obstructive sleep apnea (OSA) can be a major surprise for most people. It can be abrupt when you’re in a conversation with a physician about snoring and excessive daytime sleepiness (EDS), and suddenly you’re a patient under care for a chronic breathing disorder. Doctors often need to address the immediate question, “What is obstructive sleep apnea?”
Sleep apnea is associated with conditions like diabetes, heart disease, stroke, obesity and high blood pressure. A Wisconsin sleep cohort study, which used in-lab sleep testing, showed that the prevalence of OSA was 9% for women and 24% for men in a sampling of 602 adults between 30 and 60 years of age. This study was also able to make the link between untreated OSA and a negative impact on quality of life in this patient population.
Treatments for sleep apnea are few; they include lifestyle changes like weight loss, continuous positive airway pressure (CPAP), oral appliance therapy (OAT), or invasive procedures like maxillomandibular advancement surgery (MMA). Understanding sleep apnea as a disease requires an understanding of the mechanics of respiration and basic anatomy of the upper airway. This article will discuss how sleep quality is impacted by this condition, as well as what you can do to help prevent the negative health consequences of OSA.
Understanding Obstructive Sleep Apnea
Mechanics of Respiration
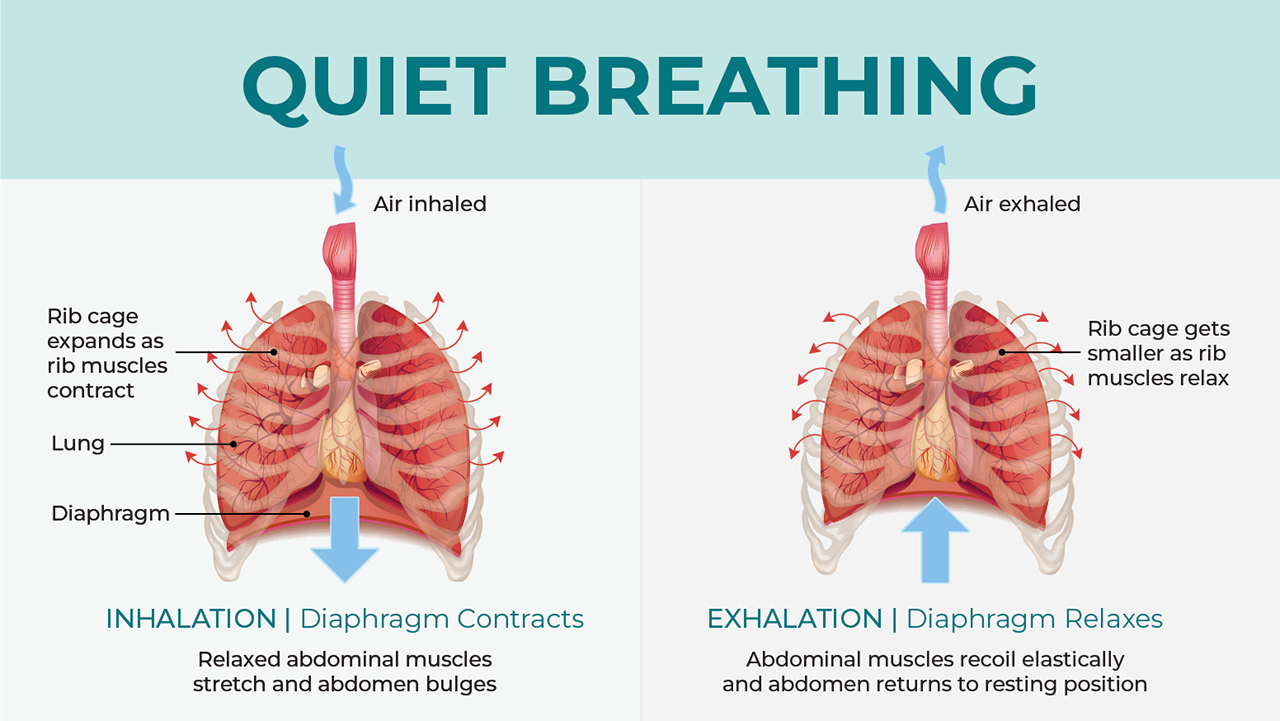
Breathing is composed of two parts: mechanical ventilation, which uses the muscles of the diaphragm and intercostal muscles to pull air into the lungs; and gas exchange, which is the process of passing oxygen from air into the bloodstream and exhaling carbon dioxide. It’s estimated that the average person takes between 17,280 and 23,040 breaths a day.
Diaphragmatic breathing (aka tidal breathing) involves the amount of air that is moved in the lungs, which is called tidal volume. This does not involve the entire capacity of the lungs. There is reserve capacity that will accommodate additional demand (e.g., while running or doing other aerobic exercise).
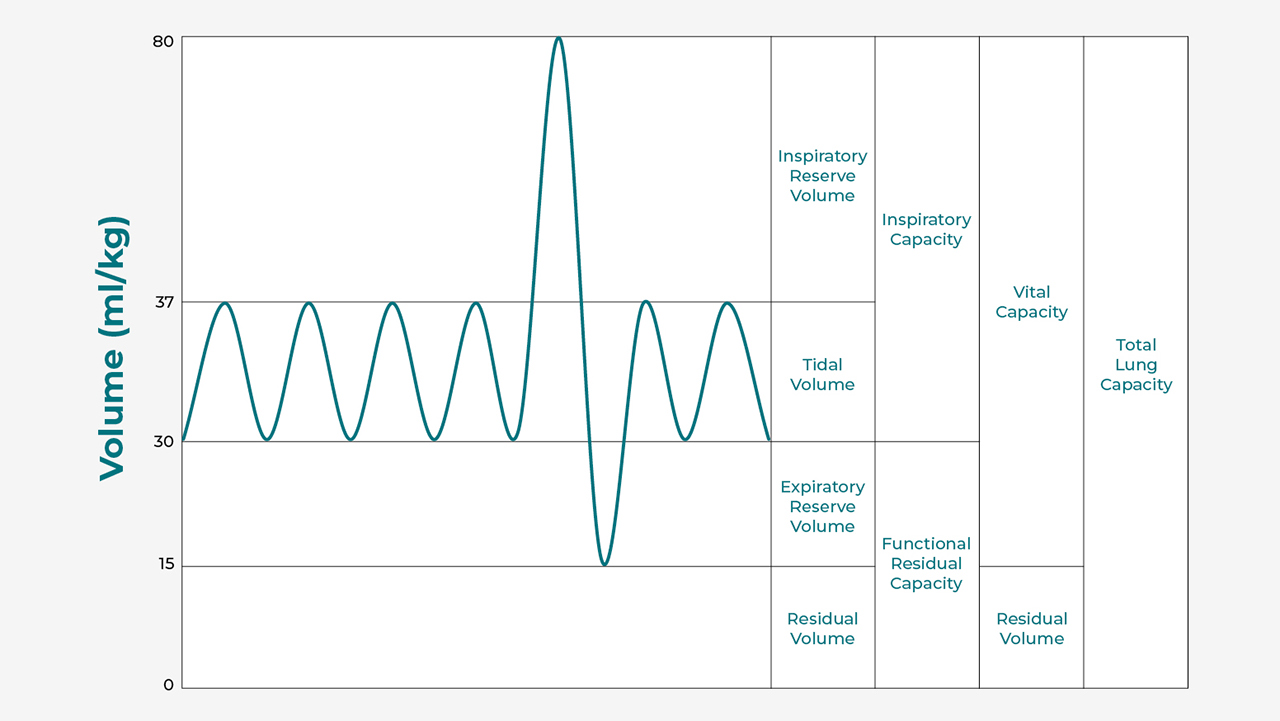
Example of tidal volume.
Source: Adapted from Kapwatt at English Wikipedia
Types of Sleep Apnea
Apnea, a Greek word that means “breathless,” can be categorized into three types:
- Obstructive apnea (OSA) — A condition where there is respiratory effort, but an obstruction interrupts airflow.
- Central apnea — A condition where there is no respiratory effort (e.g., a breath hold or a neurological interruption in respiratory drive, resulting in no airflow).
- Mixed or complex apnea — Both conditions (OSA and central apnea) exist during the same night’s sleep.
Anatomy and Physiology Involving OSA
OSA is a condition that primarily concerns the upper airway. The nasal passages, nasopharynx, oral cavity, tongue, adenoids, tonsils, oropharynx and hypopharynx are all structures that can collapse, obstruct or be obstructed in some other way to restrict breathing or increase the airway’s resistance (work of breathing). This condition commonly includes loud snoring, and the sleep disruption it creates causes sleep fragmentation, which results in excessive daytime sleepiness.
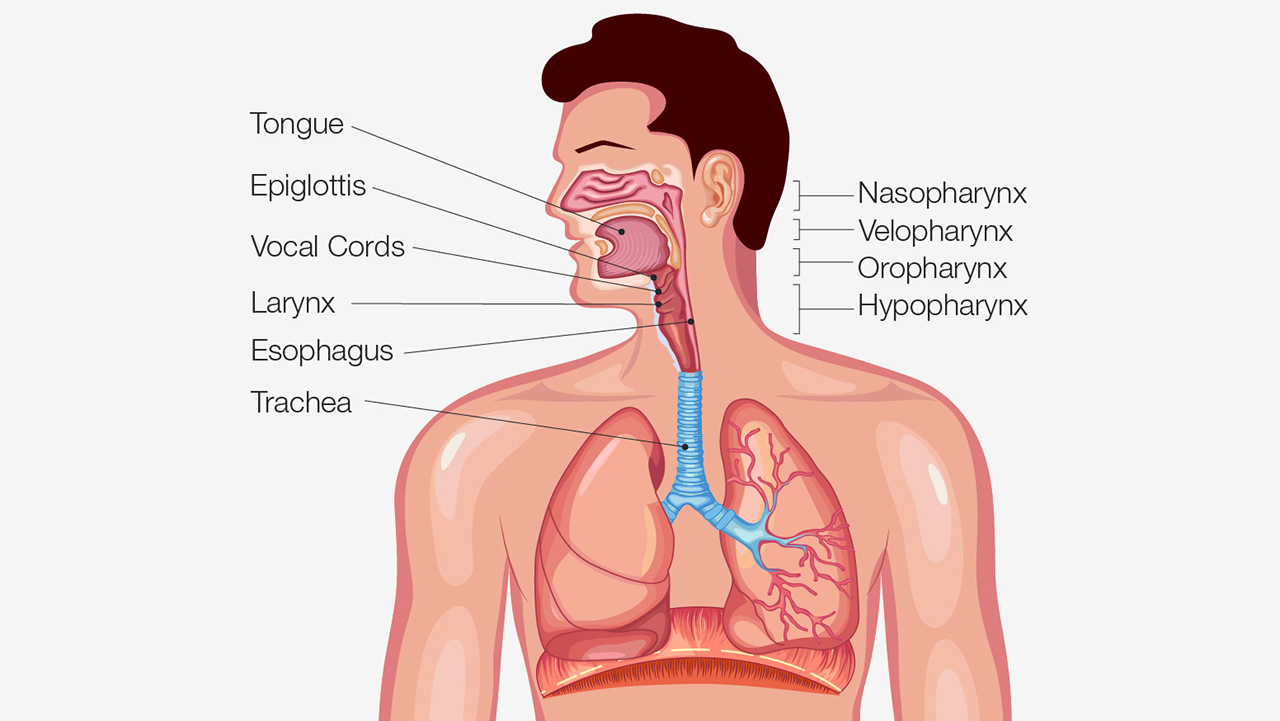
Anatomy of the airway.
Most quiet breathing is through the nose. Nasal breathing is very important because the nose has a small volume where air can be warmed, moistened and filtered with thick, sticky mucus, before being delivered via the trachea to the lungs.
During sleep, the physiology of the airway changes. For example, tissues relax and respond differently to airflow and respiratory effort. The tongue forms most of the wall of the pharynx. Changes in muscle tone, either stiffening or relaxing, affect the shape, size, and collapsibility of the oropharynx and the velopharynx.
When relaxed during sleep, the jaw falls open and the tongue drifts back against the posterior wall of the oropharynx and hydrostatically adheres to the thick mucus in the throat, forming a seal and obstructing the airway. The chest walls and abdominal muscles continue to try to move air in and out of the lungs; however, with the airway blocked, negative pressure builds until the patient gasps awake, restoring tone to the tongue so that the patient can get a few gasps of air before repeating the process a few breaths later.
How Sleep Quality Is Impacted
In order to demonstrate the impact of upper airway dimension and caliber on breathing during sleep, you may try the three exercises shown below. They will help you understand the difference between upper airway resistance syndrome, snoring and obstructive sleep apnea. If you find them compelling, you may decide to incorporate these exercises into your patient or dental team education.
Exercise 1: Upper Airway Resistance Syndrome
- Take a moment to breathe quietly.
- Allow your jaw to relax and your airway at the base of your tongue to close slightly.
- Don’t make the snore sound, but feel the resistance build.
This is upper airway resistance syndrome (UARS). It’s not a clinical condition, but the effect of increased effort can affect sleep quality, leading to fatigue and unrefreshing sleep. These shallow breaths can be scored in a sleep lab as hypopnea, a sequence of shallow breaths for 10 seconds or longer while asleep when airflow is at least 30% lower than normal (see below).
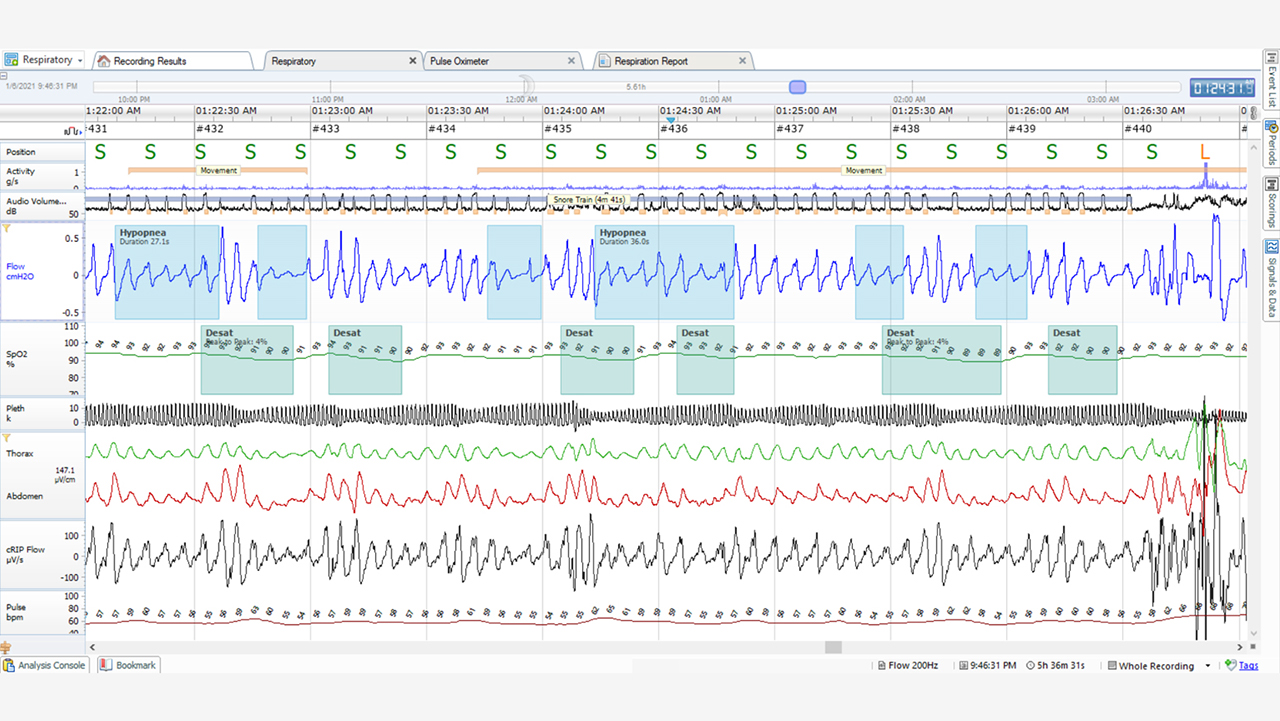
This chart, courtesy of Nox Medical, shows information from a Noxturnal® analysis recorded during sleep. The blue boxes indicate airflow that has dropped by 30%. The slightly out-of-phase green boxes indicate drops in Sp02 (arterial blood oxygen) that is related to the previous episodes of shallow breathing or hypopnea.
Exercise 2: Simple Snoring
- While your airway is in the UARS position, allow the pressure to build until the snoring sound begins. You should feel the extra effort to draw a breath.
- Feel the vibration of the tissues of the upper airway.
- Change the position or tone of the tongue, and notice that changing this position changes or alleviates the snoring sound.
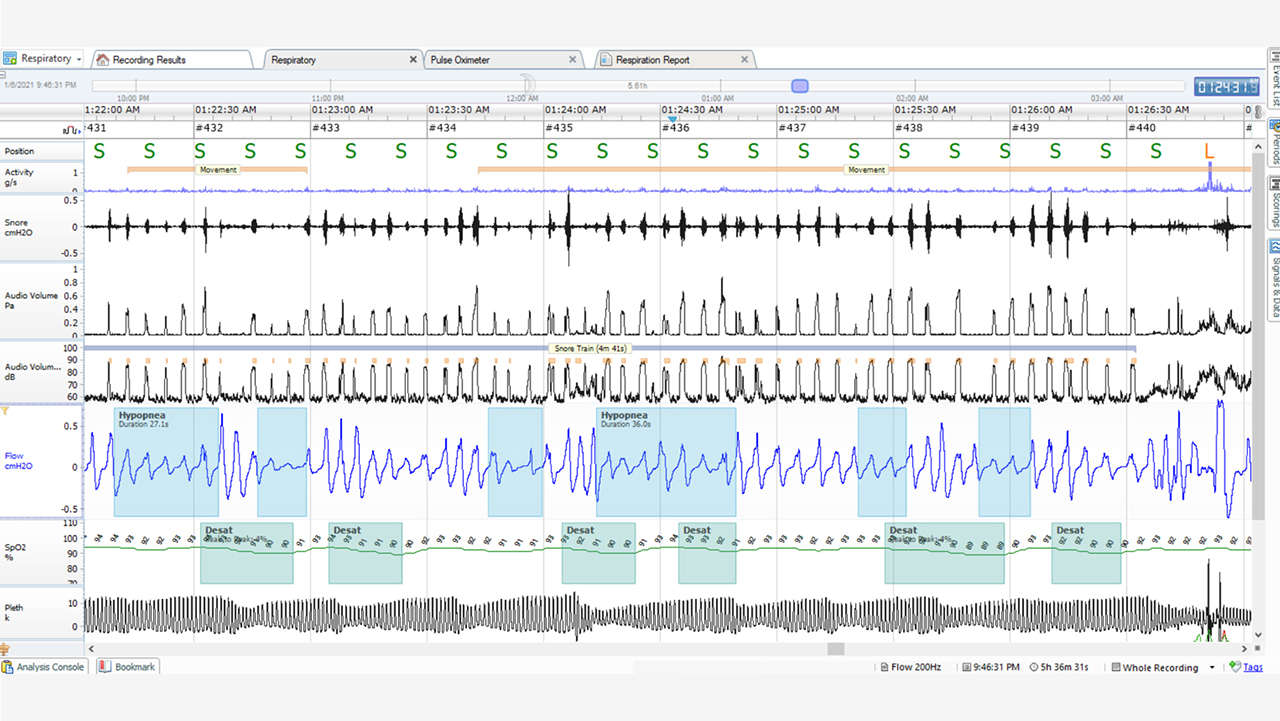
This chart from Nox Medical shows that scored snoring (small yellow marks) indicate snoring. Blue blocks indicate shallow breathing or hypopnea, and the green signals indicate drops in Sp02 (arterial blood oxygen) that is related to the previous episodes of shallow breathing or hypopnea.
Some dentists use a variation of exercise No. 2 for finding the optimal starting position for a mandibular advancement device (MAD). It is considered by some to be helpful to have the patient make a snoring sound, and then, by advancing the mandible forward, pick a clinical start point based on the patient’s ability to make the snore sound.
This, of course, is not an exact science because tissue tone, location and response to therapy is different when the patient is asleep. The adjustability of MADs ranges from 6 mm in the case of a Silent Nite® Sleep Appliance all the way up to 15 mm for a TAP® appliance, allowing for fine titration as needed for therapy.
Exercise 3: Obstructive Sleep Apnea
- While you are snoring, allow your airway to obstruct, but keep trying to breathe.
- Feel the pressure changes in your chest. You may feel some adhesion of the pharynx.
- If you start this exercise at the end of exhalation, you will feel the physical implications of OSA in a very short amount of time. Remember that apnea is characterized by a cessation of airflow for 10 seconds or more, and some patients experience episodes for a full minute or more.
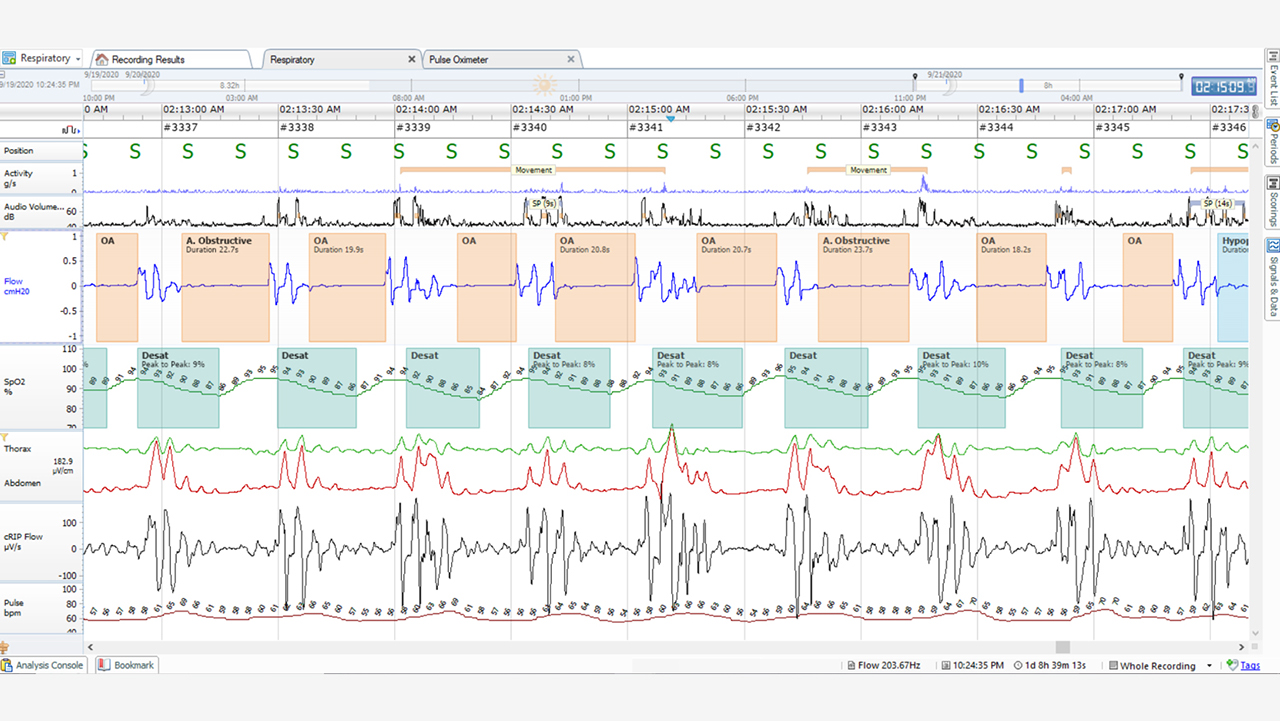
This chart from Nox Medical shows the breathing pattern of a sleeping patient in the supine position (on the back). Each segment is 30 seconds. There is the absence of airflow (in the tan-colored field) with a decrease in Sp02 (arterial oxygen saturation; in green) and corresponding respiratory effort (indicated in black and red lines). Notice that the airflow stops, then the Sp02 drops a few seconds later.
Oftentimes, patients are unaware that they have obstructive sleep apnea. When they seek treatment, the primary complaint is snoring or, if the condition is severe, they may complain of excessive daytime sleepiness. OSA can negatively impact sleep quality and overall health; therefore, treatment can be life-changing.
Watch this video to learn more about how sleep apnea affects breathing.
Conclusion
Breathing is an ongoing 24-hour activity. It is clear that the physiological response to sleep affects the tone, shape and dimension of the upper airway, which affects sleep quality. In general, patients are unaware of the impact that their snoring has on their overall health. When patients seek treatment, the primary complaint is snoring or, if the condition is severe enough, they complain of excessive sleepiness. Simple exercises can show patients what happens in the airway during sleep and help them understand the available solutions.
To discover the simple, three-step process to screen and treat patients for snoring and sleep apnea, visit glidewell.com/pmad.
More to Know
Dental CE
- Free online CE course by Mark E. Abramson, DDS: “Introduction to Dental Sleep Medicine”
Send blog-related questions and suggestions to hello@glidewell.com.





