Replacement of a Maxillary First Molar: Extraction, Socket Grafting and Sinus Lift

Following tooth extraction, the natural process of bone healing results in a loss in width and height of the supporting hard tissue. In the posterior maxilla, the proximity to the maxillary sinus provides additional challenges in areas of decreased bone volume. When teeth are present, the roots act like tent poles holding up a circus tent — but once the tent poles are removed, the tent itself will fall. This results in the loss of vertical height of bone in an area of the mouth that has the lowest bone density and takes on most of the occlusal forces. Because maintaining that height of bone is important in positioning the dental implant, grafting the socket becomes a critically important technique.
Bone grafting is possible because bone tissue, unlike other tissues in the body, has the ability to regenerate completely if provided adequate space. Grafting at the time of extraction minimizes bone loss, supports soft-tissue structures, and provides an adequate site for implant placement in 12–16 weeks. Failure to graft can lead to soft-tissue infiltration in the socket, loss of ridge height and width, and 30%–60% bone loss in a three-year period.1,2,3 As natural bone grows, it will generally replace the graft material completely, resulting in a fully integrated region of new bone.4,5
For socket regeneration, a two-in-one technique using the OsteoGen® Plug (available through Glidewell Direct; Irvine, Calif.) can achieve successful sinus tenting in preparation for a dental implant. In most cases, utilizing this material eliminates the need for a membrane. The OsteoGen Plug is an excellent, safe material to use, particularly when all walls are maintained following surgical extraction of nonrestorable teeth.
KEY MATERIAL CHARACTERISTICS FOR SIMPLIFIED SOCKET GRAFTING
OsteoGen Plugs have made socket grafting in preparation for dental implants simple, predictable and cost-effective for the dentist and patient alike. An alloplastic graft, the plug is a resorbable calcium apatite crystal cluster with bovine Achilles tendon collagen. It is bioactive, controls invagination of soft tissue and forms a strong bond with bone as it resorbs. The clusters are packed and intertwined, and form a hydrophilic matrix that absorbs blood. The graft and collagen combination fulfills two primary purposes of a membrane in socket grafting: It contains the graft material and restricts migration of connective tissue through both a physical and chemical barrier.5
The physical barrier is created as the plug is compressed down into the socket site. The chemical barrier is created as the condensed plug crystals hydrate with blood and the resorption process begins, releasing calcium ions and creating an environment favorable to bone and not soft tissue.
As natural bone grows, it will generally replace the graft material completely, resulting in a fully integrated region of new bone.
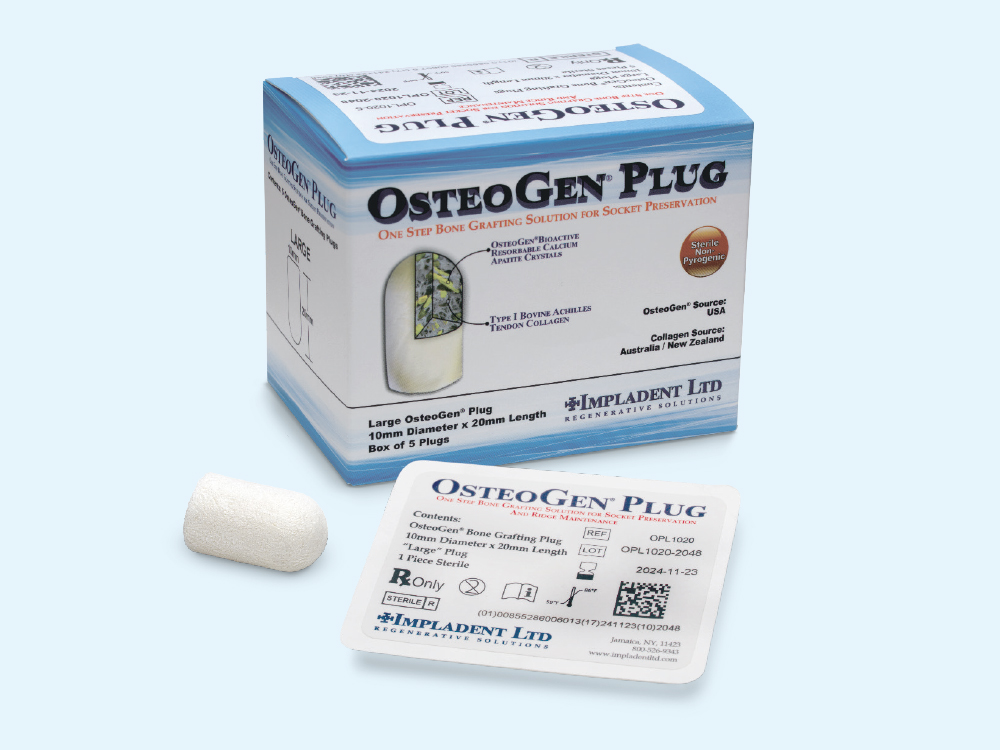
In most cases where all socket walls are maintained, the OsteoGen Plug functions as a two-in-one solution, eliminating the need for a barrier membrane. The plug will be radiolucent on the day of placement. As the crystals are resorbed physiologically by osteoclasts, osteoblast activity will replace the material with the host bone. The site then becomes radiopaque, allowing the practitioner to objectively determine bone turnover radiographically.
CASE REPORT
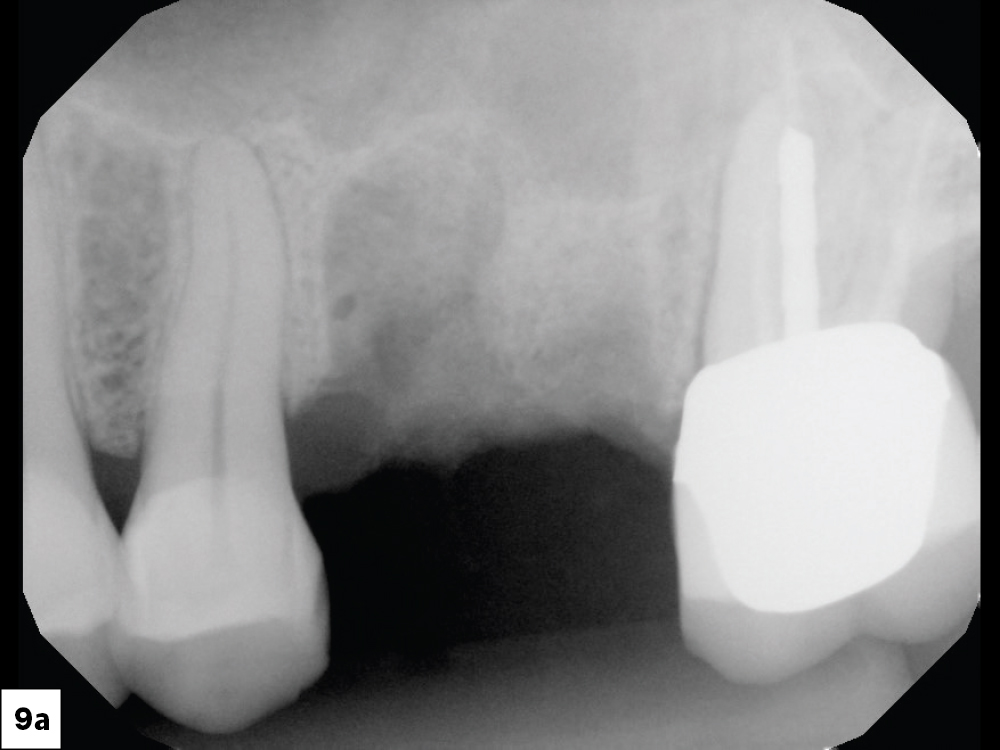
Figure 1: Preoperative digital radiograph of an endodontically treated maxillary first molar with a hopeless prognosis.

Figure 2: Using Physics Forceps® (GoldenDent; Roseville, Mich.), the tooth was removed with minimal trauma to the bone structure.

Figure 3: The divergent roots of the tooth were removed in total with minimal force.

Figure 4: The socket was evaluated for any granulation tissue, which is removed with a sharp curette.

Figure 5: A sterile OsteoGen Plug was chosen for this site. The plug consists of a non-ceramic bone graft in a type 1 bovine Achilles tendon collagen matrix.

Figure 7: A physical barrier was created as the plug was compressed down into the socket site. Note that firm compression is necessary, but not as hard as condensing amalgam. The compression gives the epithelium cells two options: fight down through the condensed plug or simply go over the top. They will follow the path of least resistance, so there is no need for the placement of an additional membrane to protect the grafted material from invagination of epithelium.

Figure 8: Vicryl sutures (RELI® REDISORB® PRO Sutures; available through Glidewell Direct) were used to secure the grafted material into place. Primary closure is not required, as epithelium will grow (0.5 mm to 1 mm per day) over the OsteoGen material, following the path of least resistance. No other membrane is required as this technique utilizes a simple, two-in-one process. Maintenance of a band of at least 2 mm of attached gingiva on the facial aspect of the socket is important for periodontal health at implant sites. Sutures are typically removed in 7–10 days to evaluate the surgical site.
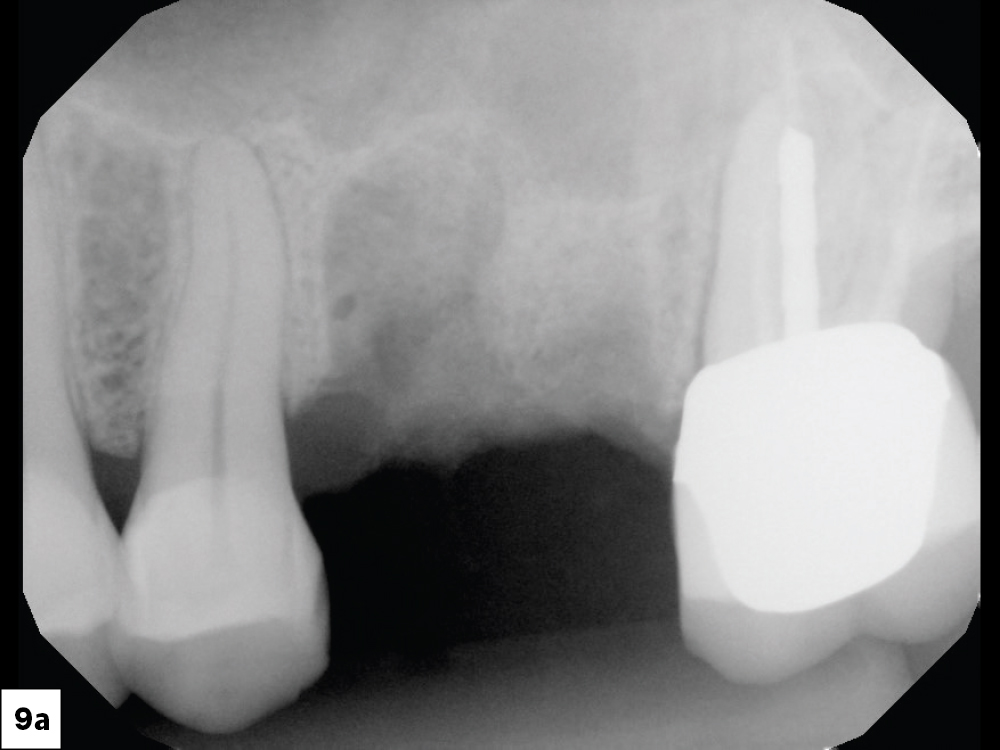
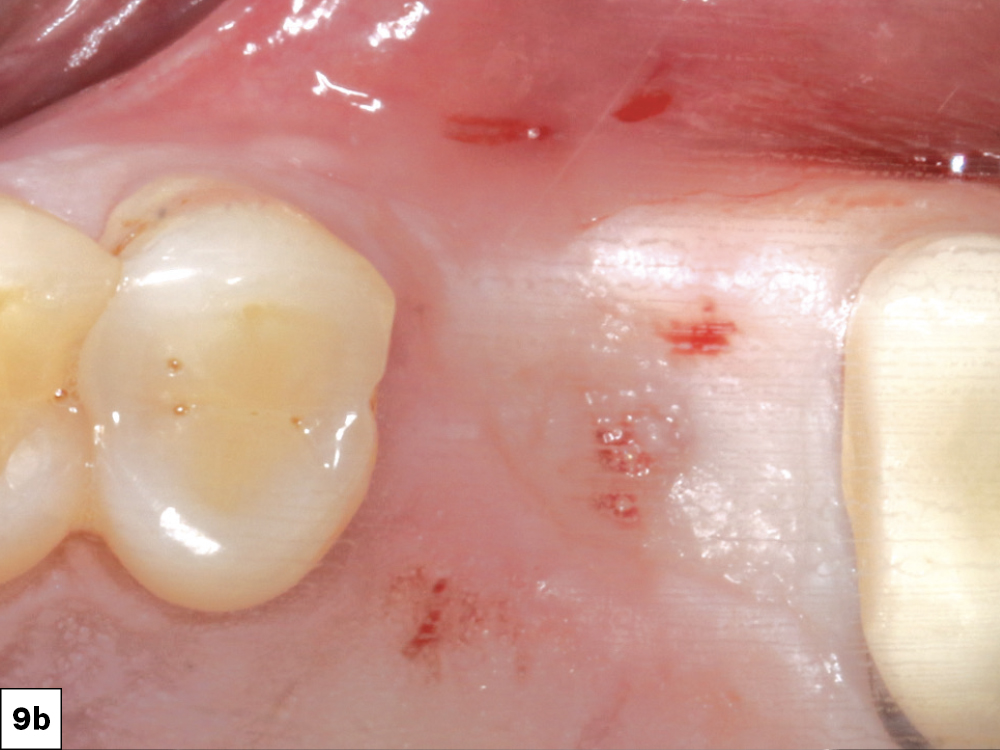
Figures 9a, 9b: After approximately four months of integration, the surgical site was evaluated. The attached gingiva position was reviewed. Local anesthetic was infiltrated to the surgical site.

Figure 10: An envelope reflection was made. No vertical incision was made to elevate the tissue facially. This minimized prostaglandin and histamine release, and reduced postoperative discomfort to the patient. The grafted site was evaluated for bone formation.

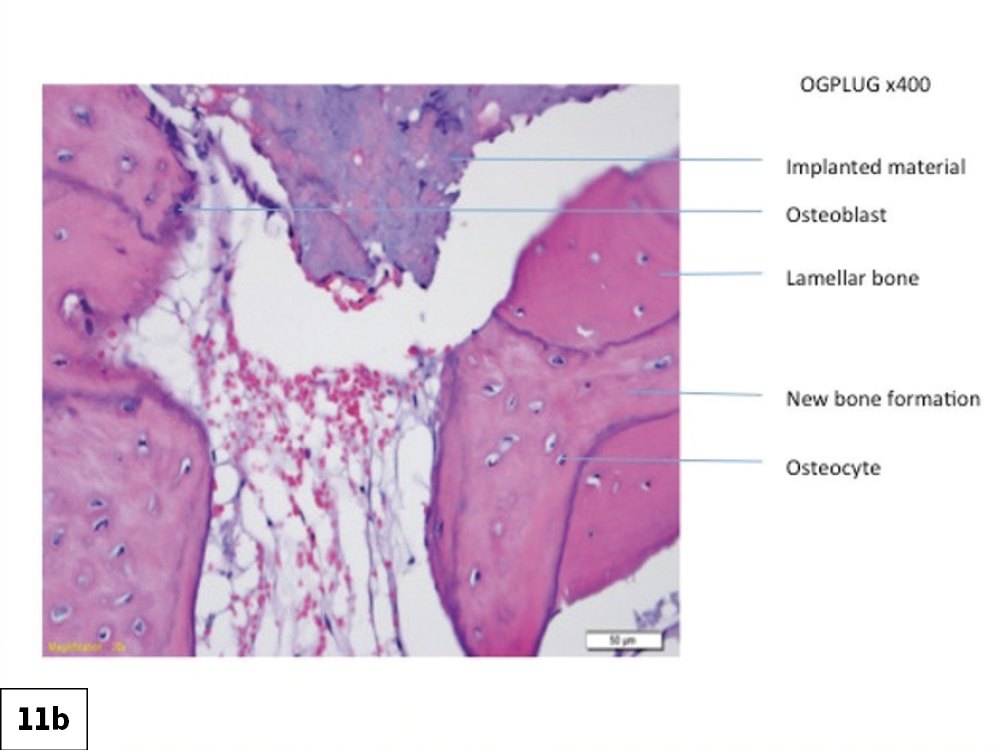
Figures 11a, 11b: Histologic evaluation of the integrated bone illustrates new bone formation in the socket site.

Figure 12: Following the surgical protocol for the Hahn™ Tapered Implant System (Glidewell Direct), a 2.6 mm pilot bur was used to establish proper angulation for the implant mesial-distally and facial-palatally.

Figure 13: Because we were focused on the maxillary sinus area, rather than using the osteotomy burs to prepare the implant site for fixture placement, I used the Hahn Tapered Implant Osteotomes (Glidewell Direct). These are shaped like the implants themselves and serve to widen the osteotomy site without bone removal, as well as compress the bone to create better initial stability. The osteotome technique also helps elevate the sinus floor to accept an implant of proper length.
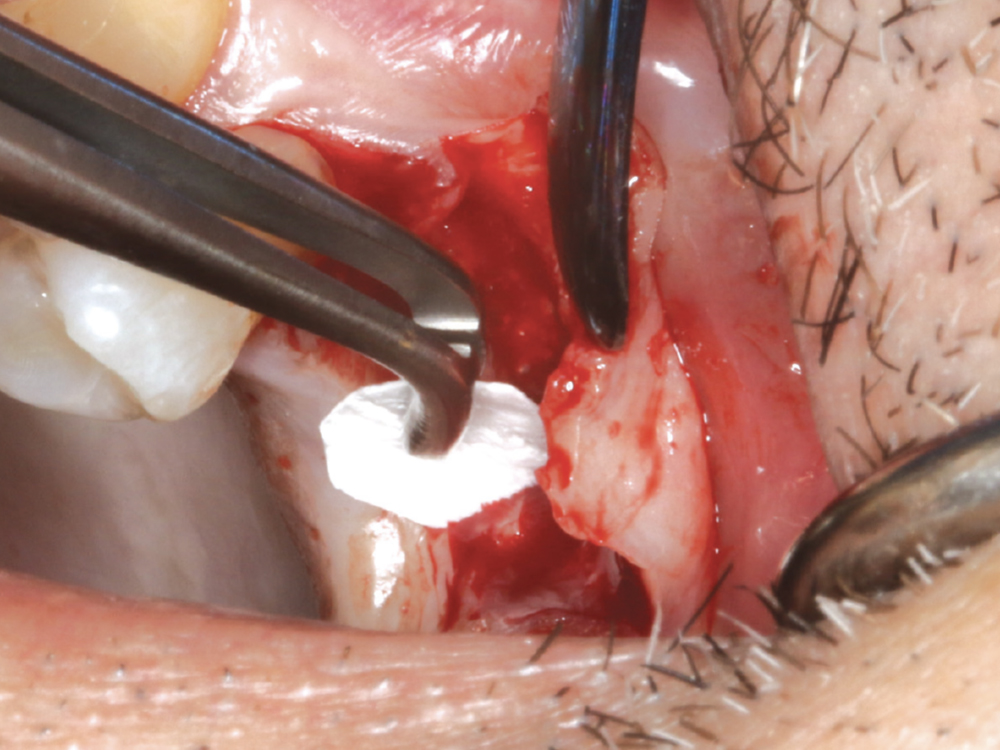
Figure 14: A rounded piece of Newport Biologics™ Resorbable Collagen Membrane (Glidewell Direct) was placed into the osteotomy site to create a new sinus floor. Another small piece of OsteoGen Plug was carefully condensed into the site to help lift the Schneiderian membrane.
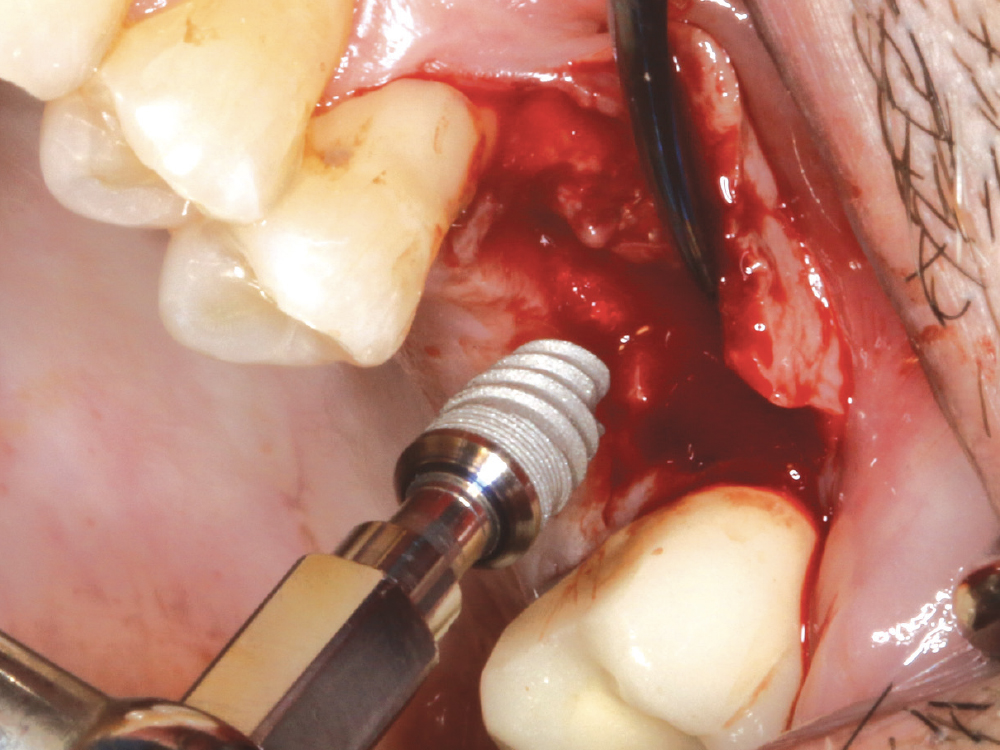
Figure 15: The Hahn implant was torqued into position at the crest of the ridge.
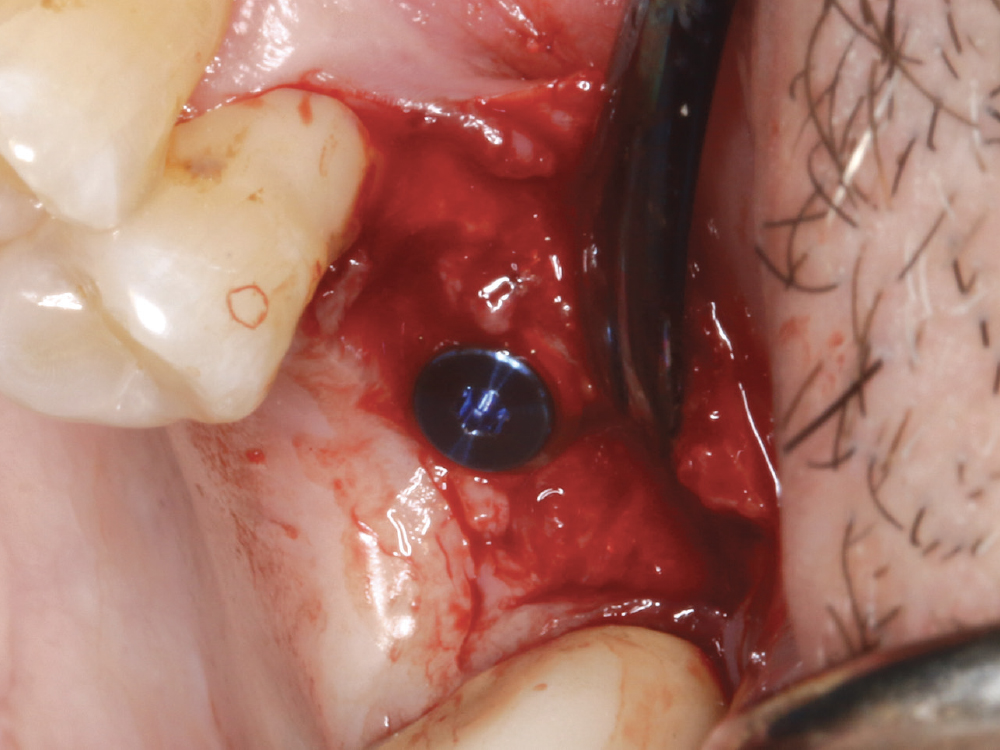
Figure 16: A cover screw was threaded into place and the site sutured to allow for uninterrupted integration of the graft and implant.
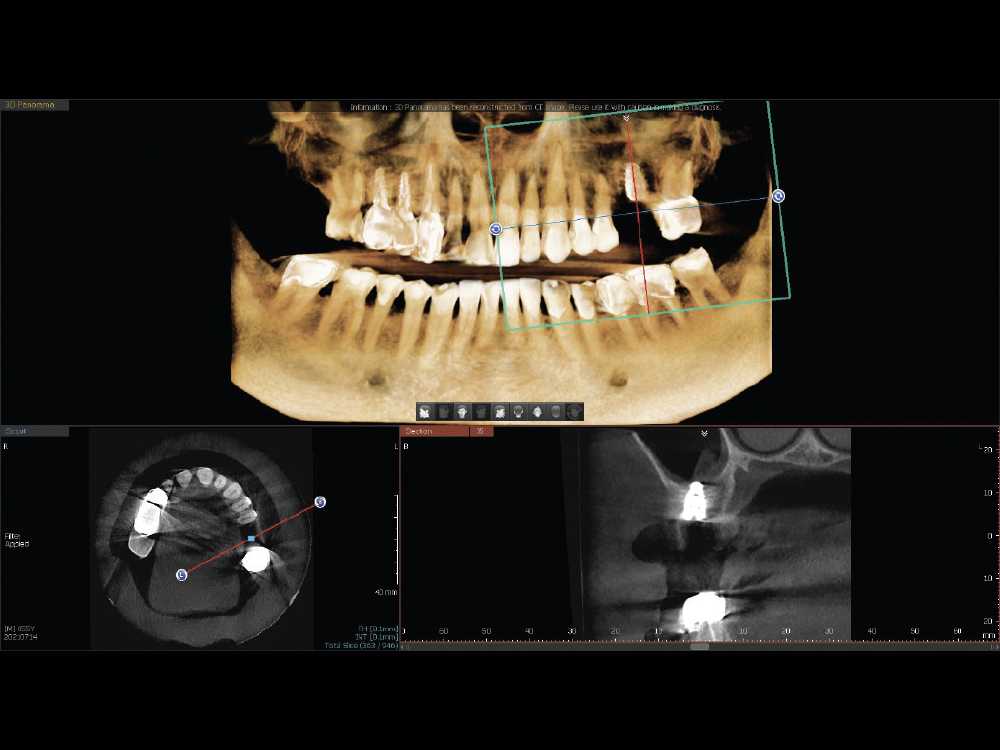
Figure 17: A postoperative CBCT analysis indicated a properly positioned implant with a sinus elevation. The successful surgical procedure ensured that the site would be ready to move forward with the fabrication of an implant-retained crown
CONCLUSION
Ridge preservation following extraction is an integral part of implant dentistry. The OsteoGen Plug is an excellent, safe option when all socket walls remain, allowing for condensation of the available hard tissue and elevation of the sinus floor to accept a properly sized implant for the resulting implant restoration.
OsteoGen is a registered trademark of IMPLADENT, LTD.
References
- ^ Kosinski TF. Innovative socket grafting techniques in preparation for dental implants. The Profitable Dentist. 2017 Summer:22-7.
- ^ Tuttle D, Kurtzman GM. Simultaneous sinus augmentation and implant placement. Inside Dentistry. 2018 Nov.
- ^ Misch CM. Maxillary autogenous bone grafting. Dent Clin North Am. 2011 Oct;55(4):697-713.
- ^ Jackson BJ, Morcos I. Socket grafting: a predictable technique for site preservation. J Oral Implantol. 2007;33(6):353-64.
- ^ Valen M, Ganz SD. A synthetic bioactive resorbable graft for predictable implant reconstruction: part one. J Oral Implantol. 2002;28(4):167-77.