Interview with Gordon Christensen, DDS, MSD, Ph.D.

There are few names more recognized and respected in the dental profession than Dr. Gordon Christensen, founder and CEO of Practical Clinical Courses® (PCC), cofounder and CEO of Gordon J. Christensen Clinicians Report®, and practicing prosthodontist in Provo, Utah. Dr. Christensen has published hundreds of articles and books and has presented over 45,000 hours of continuing education worldwide. During his discussion with Dr. Neil Park, vice president of clinical affairs for Glidewell, he explored a wide range of topics affecting the present and future of dentistry.
DR. NEIL PARK: When I went into practice 43 years ago, one of the first things I did was subscribe to Gordon J. Christensen Clinicians Report. How did you get started with this now vital newsletter?
DR. GORDON CHRISTENSEN: I was an academic at the time. I had been on numerous national and international committees to evaluate products, and I could see some challenges. And those challenges made me want to establish a nonprofit group that would allow for unbiased evaluation without money interfering, to identify the best products. When I told my peers about my idea, they said, “Oh, you’ll go bankrupt in six months.” That was 47 years ago.
NP: When you write an article for Clinicians Report, who is the reader you have in mind? Tell me about the clinician you’re thinking about.
GC: The guy or gal, working in the office, with half a dozen operatories running as fast as they can go with five or six employees wondering where their next meal’s going to come from, because of all the things we’ve all suffered through in the last several years. I think of that person who would like to get a product that works at a moderate cost.
NP: So, in those 47 years that you’ve been doing this, there have been some great products, but there have also been a few that have crashed and burned. Can you give an example of the latter?
GC: Too many!
NP: I’m thinking late ’70s, early ’80s, when the only type of ceramic we had was a porcelain crown, and there were some new ceramic crowns that came out that proved to be troublesome.
GC: Dicor, way back. We had very little research on it. Within five years, most of them had failed. So, I’m frustrated that the company didn’t do that in-the-mouth research before they started selling it.
NP: And it’s interesting, right? Because the way that the FDA clears things, basically companies just have to say that it’s substantially equivalent to something that’s already on the market.
GC: And it won’t kill you.
NP: Right. The fact that you’ve developed this scientific organization that not only clinically evaluates products, but also evaluates with benchtop testing — that’s just irreplaceable for doctors out there.
GC: I think you’re right, Neil. I was in academia for part of my career, and you need to do a certain number of papers to go from assistant professor to associate and then finally to full professor. The faster you can do that, the faster you get the promotion and more salary.
So, what are they going to do? In vivo? It takes years. They’re going to do in vitro. That’s why when you look at most of the dental journals, you see that they’re filled with in vitro studies that may not represent reality. If you add them all together and we get a meta-analysis, you know what they usually say? We need more research on this.
NP: That’s exactly what they say. And the long-term clinical trials, they’re just not there.
GC: No, they’re not. They’re not there.
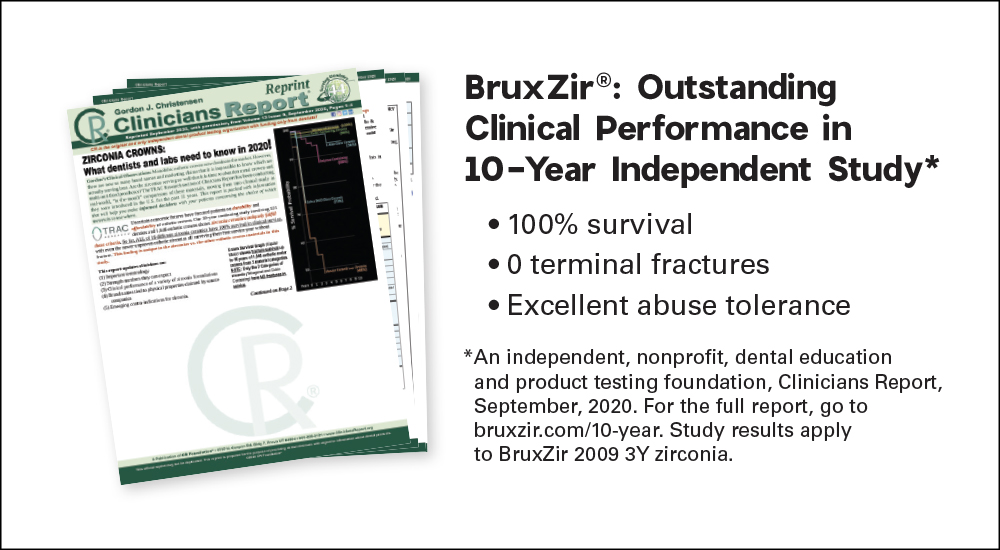
NP: Let’s talk about some of the successful products that you’ve evaluated over the years. For example, BruxZir® and Jim Glidewell’s idea to make a monolithic zirconia crown. That’s something you’ve studied over a period of years now, right?
GC: Yes. Along with my wife, Dr. Rella Christensen, the main investigator, we have studied BruxZir crowns for 11, going on 12 years, and we have periodically published our data in Clinicians Report.
NP: Based on your clinical as well as in vitro research, this massive movement that we’ve seen dentists make, from PFM being the everyday crown to now monolithic zirconia — is that a good thing for dentistry?
GC: Yes, it is a good thing. First, because the cost of making those crowns through Glidewell and other labs is lower, because of automation.
NP: And on the clinical side, it’s not a particularly difficult prep, right?
GC: Thank goodness, because BruxZir can go down to six-tenths of a millimeter thick with the original 3Y zirconia and still be adequate. It’s much like a gold crown in its tooth preparation.
NP: You’ve also been doing clinical testing on ceramic-filled composite milling materials as well, like CAMouflage® from Glidewell. What are your thoughts about that material?
GC: We did a study of numerous brand names of resin, and by the first year, nearly 30% had come off. Glidewell turned out to be the best performer of the resin crown brands with CAMouflage.
NP: So, it’s not a fracture issue, it’s debonding.
GC: Correct. They debond, apparently, because of the flexion of the material. But that has not happened to date in all the years we have been testing CAMouflage. And that’s one of the reasons why some doctors are having issues with the zirconia crowns coming off. They’re using a resilient resin cement that companies keep promoting and I keep denying works. We would rather have a more rigid cement like resin-modified glass ionomer (RMGI).
NP: Would you say RMGI is your recommendation for BruxZir crowns?
GC: Oh, absolutely no question. Eighty percent are using the 3M product, RelyX™ Luting. GC also has a similar product: GC FujiCEM® Evolve. I’m very comfortable with both.

Dr. Gordon Christensen with Dr. Neil Park in the Technologies in Restoratives and Caries (TRAC) Research clinical studies lab elaborating on a long-term zirconia crown study (in vivo).
NP: Great insights, thank you. Well, let’s move on to continuing education. One of the most important wings of your organization is Practical Clinical Courses (PCC). You’ve trained thousands of dentists; you do hundreds of courses every year. But during this whole COVID-19 experience, education has changed.
GC: Oh, did it ever.
NP: And we went more online with webinars — where do you think we are with this?
GC: Some of your readers may not know I am a Ph.D. psychologist as well as a dentist, and the psychological literature is filled with criticism of the COVID-induced virtual meetings. I did 104 virtual programs over COVID-19, and I got very tired of looking at my computer screen and wondering who was out there. We have to change that.
NP: Where are we right now?
GC: It’s going to stabilize, in my opinion, at a level where both are offered. People want to get together; they want to circulate, talk to one another, or go out and have a dinner or a cocktail. So, I do not see the live course dying. Now, I’ve been in the last year to Greater New York, Chicago Midwinter, ADA, the major programs, and people are still coming even though COVID is still threatening. They want to get together. They want to get away from their home environment. But some really like virtual courses, so we are going to have some three-hour web-based courses.
NP: When it comes to continuing dental education, what do you think is the biggest unmet need? Something that young doctors need, but they’re just not getting in some dental schools.
GC: They get almost nothing on implant placement in most dental schools. Then they get out, they take a one-day course, they think they can place implants, and no, they can’t. So that need is unmet, among others. Also, removable prosthodontics is inadequate beyond belief in dental schools now. I was in a school recently, and I asked a group of students who were ready to graduate, “How many dentures have you done?” Only one in a group of six.
NP: Why did this happen in schools?
GC: Because on came — and I’m not indicting technology — but on came CEREC®. On came a whole lot of technological things. And the companies were more than happy to provide those on-consignment items to the school, and that took time away from traditional curriculum that taught removable prosthodontics and other key topics.
NP: And, as we mentioned before, denture construction is the basis of so much other restorative dentistry. And you certainly can’t do a full-arch implant restoration if you can’t do a complete denture.
GC: No, you can’t.
NP: Do you think the answer is in technology? For example, people that purport to have digital dentures, but the idea of what you and I call the wax rims, they haven’t digitized that yet.
GC: We’re not there yet.
NP: Okay, let’s dig into implants. For many years now, you’ve talked about implant dentistry and the placement of implants being something that every general dentist should be comfortable with.
GC: I sincerely believe that — at least at the less complicated level.
NP: So, with the work that you and others have done over the years, have we now proven that a general dentist with the right amount of training and the right materials can do a competent job of implant placement?
GC: If I get someone who’s done a bit of surgery, they can put a single implant in a healthy person after taking just a first-level course. Now, as you know, the great majority of implant cases are singles. So, if they learn how to do a single, it’s not long until they would graduate to our second-level course, which is multiples. And then they’ve got to learn more about occlusion. We give a course called Comprehensive Predictable Dentistry where we go through occlusion, among many other topics.
NP: I noticed you have two cone beam machines in your clinic. Do you believe cone beam and 3D imaging is a critical part of implant dentistry?

A number of key instruments in the TRAC (in vivo studies) clinical studies lab.
GC: Currently, cone beam is in about 28% to 32% of general dentist offices. It’s the highest revenue-producing procedure they have. It’s a staff-driven procedure. It’s highly valuable for things like implant placement, difficult endodontic cases, impactions and diagnosis. For some procedures, it’s becoming standard of care.
NP: And I’ve noticed that the price of these machines has come down significantly.
GC: Yes, definitely a good investment.
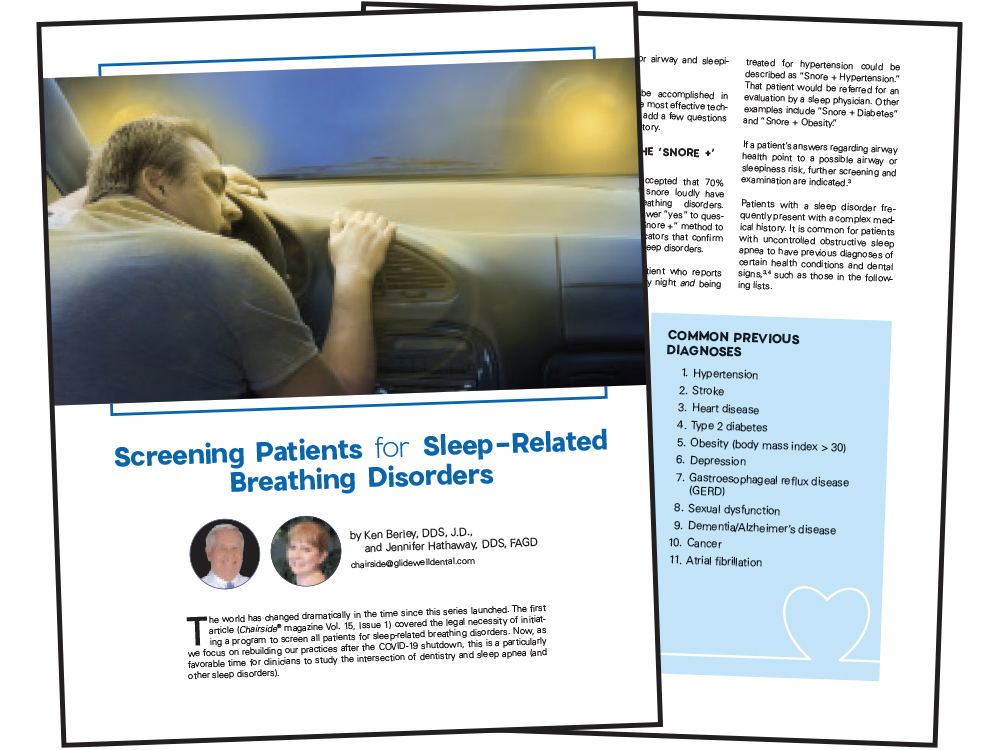
NP: Okay, let’s move on to another area of dentistry: sleep. There was a position paper from the ADA that says all dentists should be screening for sleep apnea. What are your thoughts about this area of dentistry?
GC: Forty percent to 50% of adults snore. I think there’s enormous potential for dentists to get involved.
NP: Why haven’t more dentists embraced this?
GC: Because it’s threatening, and they don’t know how to get paid for it. You get paid for it by saying, “Do you sleep around somebody who snores?” Yes. “Would you like to stop it?” Who’s going to say no? So, your insurance plan, which is really a benefit plan, will give you nothing in dentistry. If you learn some medical codes, they will give you something. On the other hand, you’ve got to either be involved with a company that can do those codes or learn them yourself, which I have done. That’s just too much of a jump for some people. But our PCC course two weeks ago given by Dr. Jamison Spencer — students eat it up. They love it once they’ve learned how to do it.
NP: One of the protocols that Jamison Spencer talks about is this provisional mandibular advancement device (PMAD). So, even though you haven’t gotten a definitive diagnosis from the sleep physician, you can still treat this patient for snoring, and you won’t be reimbursed by medical insurance, but you can still be paid by the patient.
GC: Absolutely.
NP: It’s growing, but it’s an interesting field where a small number of doctors are treating the bulk of the patients, and there’s lots of room for other dentists to get involved.
GC: Sleep medicine is like a plum just hanging there ready to be plucked.
To learn more about dental sleep medicine, read the three-part Chairside® magazine series on screening and treating patients. Visit chairsidemagazine.com.
NP: Good advice for dentists. Well, let’s go to an even bigger topic here: the adoption of digital dentistry. As you know — because we share our data with you — the number of digital impressions received by Glidewell has been growing exponentially to where we routinely receive over 100,000 scans per month. Last month, we received scans from over 14,000 different dentists, and about 50% of our total cases came in digitally.
GC: I’m sure your question is, what’s going to happen? No question, it is the future. The current scanners are good, but I would like to see some improvements. They need to be smaller, easier to use, wireless, easily sterilizable and less expensive. Medit is one example offering a nice product at a reasonable cost.
NP: In-office milling is also becoming more popular, and AI-driven technology has gotten to a point where the design part of it is very, very simple. Where are we with that technology, and where are we going?
GC: We’ve looked at your mill (fastmill.io™ In-Office Mill), and it’s great. Glidewell has done a nice job at a lower cost. A typical American dentist does about one crown per clinical day, about 250 a year. For that person, in-office milling makes sense. A person comes in, they’ve broken off an anterior, they’re going to a granddaughter’s wedding reception, and they need a crown.
NP: All right, let’s switch over to dental education. You were involved in the founding of three dental schools.
GC: Yes, in Kentucky and Colorado, and then, mainly politically at the University of Utah.
NP: So, let me ask you this: Is the dental school curriculum keeping up with current technology?
GC: Not in some schools is the candid answer. I talk to students very frequently, and a big concern on a lot of their minds is the lack of clinical experience they get. Recently, they had a list of the best dental schools in the world, and what did they base it on? Research grants.
NP: And typically, predoctoral students are not involved in that, right?
GC: That’s right. We should be helping practice through research, but right now, it’s the reverse.
NP: What are your thoughts regarding the high levels of debt that students graduate with?
GC: I did a paper with a young man from Harvard several years ago, when the average debt was about $250,000. And based on expected levels of productivity — while still having a family, a car, and a house payment — it would take 20 years to pay off. Today, the debt is much higher!
NP: And when students graduate with $400,000 to $500,000 in debt and higher, that affects their career. It’s much harder to go into private practice if you’re already coming out with this big debt.
GC: The current graduate has no place to go. You either go into corporate, or you look for an older doctor to take over his or her practice.
NP: Do you think all these financial pressures on young dentists can have an impact on the clinical decisions that they make?
GC: Are you kidding? I constantly hear from dentists in my CE courses, “This patient came in and they had 10 fillings to be done. I examined them and determined they didn’t actually have any to be done.”
NP: What would your advice be to young dentists who maybe get a little aggressive in their treatment planning?
GC: Overtreatment is not just happening in dentistry. All kinds of things like hysterectomies are being done wantonly right now that are well beyond the ethical orientation. The patient should be a part of the decision for anything that’s done, and unfortunately, they’re not sometimes. But I think ethics can be resurrected. We’re certainly going to try. We’re dentists. We chose it. We love it. Let’s now get ethical with it. But the schools have got to turn around and start educating more thoroughly on the clinical skills necessary for dental practice.

During the COVID-19 pandemic, Dr. Christensen participated in the Glidewell Online Study Club and provided vital current information for dentists navigating COVID-19. Recordings of his presentations are available at glidewell.com/webinar.
NP: I want to address corporate dentistry and the DSO phenomenon. Recently, one start-up dental school received a $32-million donation from someone who made that money starting a DSO. And then another school received $5 million from a person who started a DSO. This has got to be having some influence. Is this a dangerous situation?
GC: Well, I have written several papers on this topic, and I’ve looked at the good and the bad. They serve a place for the younger dentist who has no place to go because we’re so oversaturated. For example, Utah is so oversaturated with dentists, it’s almost impossible to start a practice. Now we’re seeing midcareer dentists who are tired of the administrative headaches of running a practice move over to DSO practices. Meanwhile, I’m seeing an opening for younger dentists where they’re not worrying about any one of the things I just mentioned, so they have a place. And some of the ones right on the top like Pacific Dental Services, Heartland Dental and Aspen Dental Management, Inc. are providing ethical practice opportunities for dentists of all ages.
NP: All these factors together — the fact that there are DSO and corporate practices that will employ the young dentist, and the fact that young dentists have such a high debt load — have pushed the situation so that right now the percentage of dentists who own practices has fallen to 73%. And as recently as 2005, it was 85%.

Dr. Christensen in the Practical Clinical Courses seminar room where live patients are treated, hands-on courses are conducted and educational videos are produced.
GC: Right. DSOs are not going away, but private practice is going to remain. Many patients want the personalized kind of treatment that private practice provides.
NP: Let’s talk briefly about COVID-19. You appeared on my webinar, the Glidewell Online Study Club, so many times to give all the latest advice on this topic. I really have to thank you for the research that you and Rella did to help us understand how to practice through this pandemic. You saved dentists in this country hundreds of millions of dollars because you said they did not need to get all these special air handling and air filtration devices. You tested it all.
GC: Yes, it was a major endeavor we took on. I think we had about 27 different devices. Just crazy, crazy stuff. Some doctors would put a half dozen of those big, tall air purifiers in their office costing $1,000 or $2,000 each. Nonsense.
NP: Will there be any lasting changes in dentistry because of this pandemic?
GC: No. People were saying you’ve got to have this, you’ve got to have that, you have to cover everything. It’s now post major-COVID, and most have already gone back almost exactly to where we were before.
NP: And how about you, Gordon? What does the future hold for you?
GC: Well, I was in for a physical recently, and I said, “How long will I live?” He said, “Well, my data says 106.” So, I’ve got a ways to go. Now, I’m not slowing down, but we’ve brought in Dr. Mark Durham to help with research and some administrative duties so that I can devote my energy to what I do best, and that’s teaching.
NP: Dr. Durham is a prosthodontist?
GC: Yes, and he has a presidential endowed chair at the University of Utah, in honor of Rella and me. He’s really doing great work, both at Clinicians Report and at the dental school.
NP: Gordon, they say if you want something done, ask a busy person. In my career, anytime I’ve ever needed your help, you never said no. You’ve always been there. It’s always our honor to be associated with you, and we look forward to many more years of working together.
GC: Thank you. I would say that about Glidewell, too, because when we’ve been doing research projects, Glidewell has been more than willing to cooperate and help us with whatever we wanted to study. It’s been a great partnership.
All third-party trademarks are property of their respective owners.